Prescription Overview - FLORIDA BLUE
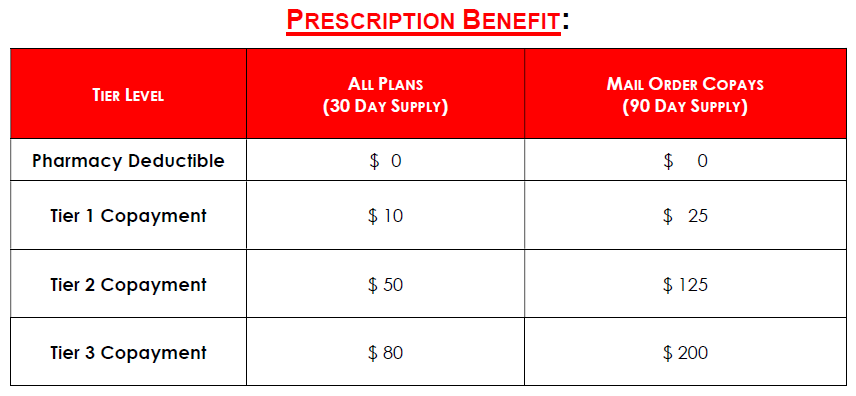
The FLORIDA BLUE group plans include a prescription drug benefit that features a tiered structure. This offers you more flexibility when making decisions about your prescription drug purchases.
COPAYMENT PER PRESCRIPTION ORDER OR REFILL: Your Copayment is determined by the tier FLORIDA BLUE has assigned the Prescription Drug Product. All Prescription Drug Products on the Prescription Drug List are assigned to Tier 1, Tier 2, Tier 3. Please access www.FLORIDABLUE.com, or call the Customer Service number on your ID card to determine tier status.
For a single copayment, you may receive a Prescription Drug Product up to the stated supply limit. Some products are subject to additional supply limits. All prescription drugs must be obtained from a Plan Retail Network Pharmacy or Plan Home Delivery Network Pharmacy and must be medically necessary for the care and treatment of an illness or injury.
RETAIL NETWORK PHARMACY: Prescription drugs may be dispensed up to a 30-day supply by a retail Plan pharmacy. Oral contraceptives may be dispensed for up to three cycles (upon payment of three copayments).
HOME DELIVERY NETWORK PHARMACY: Prescription drugs may be dispensed up to a 90-day supply by mail-order pharmacy.
To Access the Medication Guide online, visit:
https://www.floridablue.com/members/tools-resources/pharmacy/medication-guide
Then scroll to: Employer Large Group Plan Name, click on BlueOptions, Open Guide